Oct 14, 2015 | Newsletter Archives
In this Issue:
NJNI Grantees Put New Focus on Population Health in Nursing Curricula
NJNI’s Collaborative Learning Community Director to be Honored as a “Living Legend”
New Jersey Action Coalition Summit for Nurses to Focus on ‘Building a Culture of Health through Innovation’
Nurses On Boards Coalition Seeks Participants
Alumni and Scholars Update
Did You Know…?
NJNI Grantees Put New Focus on Population Health in Nursing Curricula

Nurse educators use funds to prepare students to provide care in our rapidly changing health care system.
Three New Jersey nurse educators are giving nursing education a makeover.
New Jersey nurse faculty members Robert Scoloveno, Cheryl Holly, and Katie Hooven are leading efforts at their schools to redesign nursing curricula so students will be better able to provide care in a system that is undergoing rapid change.
Their primary goal is to fill curricular gaps relating to population and community-based health so students get a “bigger-picture” understanding of health and health care and are prepared to provide care in community-based settings, where it is increasingly being delivered. The work is funded by grants from the New Jersey Nursing Initiative (NJNI), a program of the Robert Wood Johnson Foundation that is working to transform nurse education in the Garden State.
Traditional nursing curricula tend to emphasize hospital-based “sick” care for people with acute illnesses or injuries, nurse educators say. It needs more emphasis on community-based care to reflect changes in care delivery patterns as the population ages and as the number of people with chronic conditions rises. Nursing schools must also put more focus on population health so students better understand and are more able to take steps to reduce health disparities, they say.
“We looked at our curriculum and we saw that a lot of the focus was on clinical experiences that involve patients with acute illnesses,” said Scoloveno, PhD, RN, CCRN, an assistant professor of nursing at Rutgers University in Camden. “We were training our nurses to be very skilled clinicians, but we really weren’t giving them experiences that enabled them to see the bigger picture in terms of the population and communities around them.”
Filling Gaps
To address that gap, Scoloveno and his colleagues applied for and won an NJNI grant to build a school-based, nurse-managed health clinic at a nearby charter school that serves low-income families. The clinic, which opened in September, provides students with comprehensive primary care services and gives nursing students opportunities to gain clinical experience in delivering community-based care. Nursing faculty are also using grant funds to weave population health into their coursework.
“Skill-based learning is a big part of our curriculum, but we also want to give students a bigger-picture look at health,” Scoloveno said. “When we have an adolescent at risk for obesity or diabetes, for example, students are taking a step back and thinking about what factors, other than genetics or socioeconomic status, might contribute to the condition. There’s a broader scope right off the bat. I can see our whole landscape changing in terms of how we educate students.”
Also at Rutgers, Cheryl Holly, EdD, RN, ANEF, one of the nursing school’s associate deans, is overhauling the curriculum so it better addresses elder care. She and her colleagues are creating new simulation activities that teach students to screen elderly patients for depression, for example, and prevent errors that can arise when older patients are prescribed multiple drugs. They are also partnering with elder-care facilities to give students new clinical experiences in geriatric care. The changes are slated to take effect in the spring.
“Working with older people is not a very highly desired career option for nurses,” Holly says. “We’re hoping that incorporating some exposure to elderly patients in communities and changing the discussion to focus on healthy elderly wellness—rather than chronic disease—might change students’ opinions.”
At the College of New Jersey’s School of Nursing, meanwhile, Clinical Site Coordinator Katie Hooven, MSN, MBA, RN, is using the NJNI grant to integrate population and community health—particularly informatics and technology, systems-based practice, and quality improvement—into the entire curriculum. Hooven and her colleagues are also creating new clinical experiences in community health and training faculty to teach population health.
“Health care in general is going to be more focused on primary care prevention, and a lot of services will be provided outside of hospitals,” Hooven said. “If 70 percent of students’ clinical experiences are in acute care settings, we’re not preparing them for the real world or for the jobs they will be getting.”
Learn more about NJNI at www.njni.org.
Back to Top
NJNI’s Collaborative Learning Community Director to be Honored as a “Living Legend”

Diane Billings, EdD, RN, FAAN, who directed the New Jersey Nursing Initiative’s (NJNI) Collaborative Learning Community (CLC) from its inception, will be honored this month by the American Academy of Nursing as one of just five Living Legends. Designation as a Living Legend is the Academy’s highest honor.
According to the Academy, Billings is being honored “for her legendary work to improve how faculty teach and prepare their students to provide safe and high quality care to patients. She has shaped the national agenda for nursing education by developing and testing best practices for teaching; by building capacity for adoption of best practices in teaching through her service to nursing organizations; and by advancing the science of nursing education.”
The CLC was an integral part of NJNI’s Faculty Preparation Program, which ended this year. It supported the 61 New Jersey Nursing Scholars in their master’s or doctoral programs, through webinars, learning sessions, annual meetings, and an online network. The CLC also helped lay the groundwork for NJNI’s current focus on what and how nurse faculty teach the next generation of nurses.
The other nurses being honored as Living Legends this year are:
Marylin J. Dodd, PhD, RN, FAAN
Fannie Jean Gaston-Johansson, PhD, RN, FAAN
Marie E. Manthey, MNA, PhD (hon), FRCN, FAAN
Afaf I. Meleis, PhD, DrPs (hon), FAAN
“The Academy is honored to designate these five individuals as Living Legends for their far-reaching and sustained impact on nursing, health and health care,” said Academy President Diana J. Mason, PhD, RN, FAAN. “They are stellar examples of nurses’ commitment to and excellence in promoting the health of people.”
The Academy’s board of directors recognizes a small number of fellows as Living Legends each year. To be eligible, a Living Legend must have been an Academy fellow for at least 15 years and have demonstrated extraordinary and sustained contributions to nursing and health care throughout their careers.
“We are delighted to see Diane Billings honored as a Living Legend,” said Mary Joan Ladden, PhD, RN, FAAN, senior program officer at the Robert Wood Johnson Foundation. “Without her, the NJNI would not have been nearly as successful in preparing nursing faculty to not only educate the next generation of nurses in New Jersey, but to use innovative techniques in the classroom and to see themselves as leaders. Her commitment to the program and to nursing education has been an inspiration to us all.”
Back to Top
New Jersey Action Coalition Summit for Nurses to Focus on ‘Building a Culture of Health through Innovation’
Next month, the New Jersey Collaborating Center for Nursing (NJCCN), the New Jersey Action Coalition, the New Jersey Health Initiative and the New Jersey Nursing Initiative will hold a day-long summit on how nurses in the state can help build a Culture of Health through innovation.
The event will be held at the Forsgate Country Club in Monroe Township on Thursday, October 29. It will feature Susan B. Hassmiller, PhD, RN, FAAN, senior adviser for nursing at the Robert Wood Johnson Foundation; Lynn Fick-Cooper, MBA, and Ancella Livers, PhD, of the Center for Creative Leadership; and Toni Lewis, MPH, County Health Rankings and Roadmaps coach for the state of New Jersey.
A panel of experts will discuss how nurses are building a Culture of Health in New Jersey, and provide specific examples of successful programs. Attendees will also hear about funding opportunities.
Nurses from all health care settings are strongly encouraged to attend and participate in this important event. Attendees will have the unique opportunity to participate in informational and interactive sessions conducted by health care leaders and focused on how nurses can act on the local level to meet health care challenges in their communities and across the state. NJCCN is the lead organization in this partnership of health care groups.
For information on how to register and additional details, please contact Allison Creary at 973-353-2715 or acreary@sn.rutgers.edu.
Back to Top
Nurses On Boards Coalition Seeks Participants
The New Jersey Action Coalition (NJAC) is actively participating in the Nurses On Boards Coalition, a national effort spearheaded by the Future of Nursing: Campaign for Action and a number of nursing associations to increase nurses’ presence on corporate and non-profit health-related boards of directors throughout the country. NJAC now has an online form to collect professional information about nurses who are interested in serving on boards (governing boards, community/civic boards, school boards or others) in NJ. Nurses who are interested in serving on a board are encouraged to visit https://Bit.ly/boardserviceapplication, complete the form, and upload their resumes. All information will be kept confidential. For more information or questions, please contact the New Jersey Action Coalition at info@njactioncoalition.com.
Back to Top
Scholar Updates
 On September 21, Katherine Hinic, RN, PhD, (Seton Hall University 2015), presented her dissertation research, “The Relationships Among Perceived Stress, Birth Satisfaction, and Breastfeeding Self-Efficacy in Early Postpartum Women,” at Morristown Medical Center’s Nursing Research Day.
On September 21, Katherine Hinic, RN, PhD, (Seton Hall University 2015), presented her dissertation research, “The Relationships Among Perceived Stress, Birth Satisfaction, and Breastfeeding Self-Efficacy in Early Postpartum Women,” at Morristown Medical Center’s Nursing Research Day.
Hinic is an assistant professor in the graduate department of nursing at Seton Hall University.
Back to Top
Did You Know…?
Back to Top
May 4, 2015 | Newsletter Archives
In this Issue:
A Healthier Future for New Jersey
A Fond Farewell to the Collaborative Learning Community
Alumni and Scholars Update
Did You Know…?
A Healthier Future for New Jersey
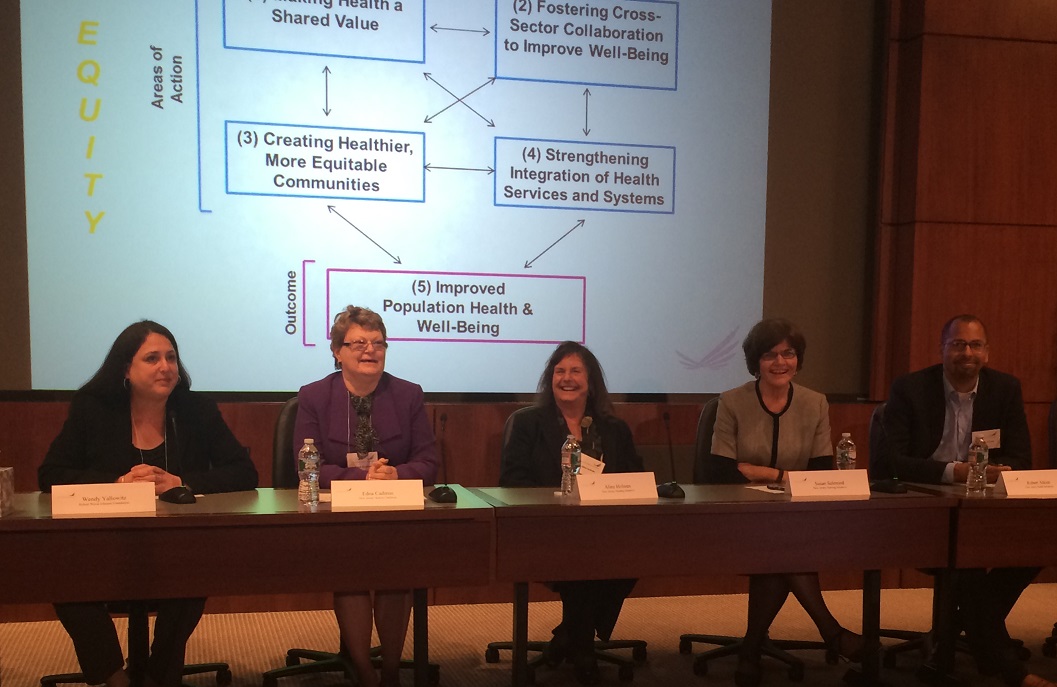
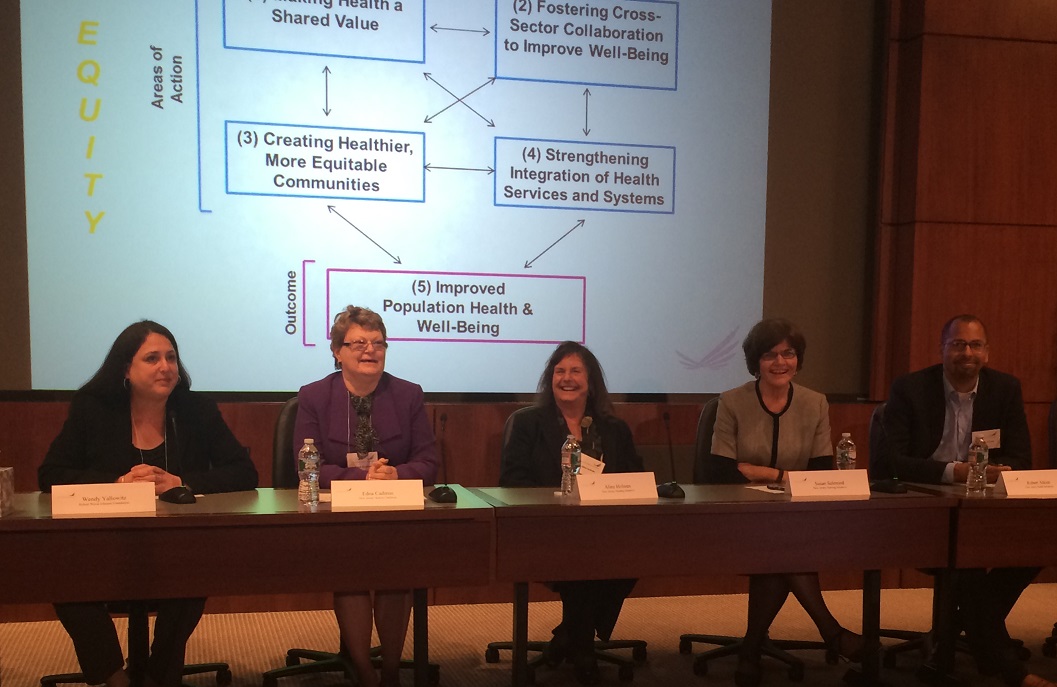
- From left to right, panel discussion moderated by Wendy Yallowitz, MSW, Program Officer RWJF with Edna Cadmus, PhD, RN, NEA-BC, FAAN, Co-Lead, NJAC; Aline Holmes, DNP, RN, Co-Director NJNI; Susan Salmond, EdD, RN, ANEF, FAAN, Co-Director NJNI; and Robert Atkins, PhD, RN, FAAN, Director, NJHI.
The importance of promoting healthy lifestyles—and building partnerships to achieve that objective—were themes of the sixth annual meeting of the New Jersey Nursing Initiative (NJNI), held on April 10 at the Robert Wood Johnson Foundation (RWJF).
The meeting, Coming Into Focus: The Big Picture of Population Health and the Direction of Nursing Education, drew nearly 100 attendees from nursing education, clinical practice, and philanthropy. NJNI’s mission is to be a leader in bringing the state’s academic and practice leaders together to transform nursing education to meet the health care demands of the 21st century.
“We must encourage nursing students to take an active role in population health, and an active role in wellness,” NJNI Program Co-Director Susan W. Salmond, EdD, RN, ANEF, FAAN, executive vice dean and professor at the Rutgers School of Nursing, said in introducing the first speaker of the day, Pamela S. Dickson, MBA, RWJF’s associate vice president for Targeted Teams.
Dickson discussed the Foundation’s goal to build a Culture of Health in which business, government, individuals, and organizations work together to build healthy communities and lifestyles. That goal “has changed us in a transformative way,” Dickson said. “I’m very happy you’re all partnering with us. We need all of you in order to bring this vision to fruition.”
Lights! Camera! Campaign for Action!
Susan B. Hassmiller, PhD, RN, FAAN, RWJF’s senior adviser for nursing, and New Jersey Action Coalition (NJAC) Co-Lead Edna Cadmus, PhD, RN, NEA-BC, FAAN, clinical professor at the Rutgers School of Nursing, provided national and state updates, respectively, on the Future of Nursing: Campaign for Action. The Campaign focuses on implementing recommendations from the Institute of Medicine’s (IOM’s) landmark report, The Future of Nursing: Leading Change, Advancing Health, which created a blueprint to transform health care through nursing.
As she discussed progress in meeting the recommendation to increase the proportion of registered nurses (RNs) with bachelor of science in nursing (BSN) or higher degrees to 80 percent by 2020, Hassmiller pointed out that enrollment in RN-to-BSN programs increased by 69 percent from 2010 to 2014. She singled out faculty in the audience to “thank you for what you’re doing. This progress reflects your hard work.”
Hassmiller added that nurses, who make up the largest segment of the health care workforce and spend the most time with individuals and families, “have such a key role in building a Culture of Health.”
In New Jersey, Cadmus said, NJAC has embraced “the opportunity to change the mindset about where nurses practice.” That work is reflected in initiatives such as the Action Coalition’s long-term care residency program for RNs, which is designed to improve the quality of care in long-term care facilities throughout the state. The first cohort of nurse residents, working in 15 nursing homes, completed the program this spring. A second cohort, in residence at 22 nursing homes, will complete their training in the fall. The program is supported by $1.6 million from the Centers for Medicare & Medicaid Services.
Cadmus also announced that NJAC will be conducting a survey to determine the number of nurses serving on hospital and other boards of directors. “It’s very important to get an accurate count in New Jersey,” she said. One of the IOM’s recommendations is to increase the number of nurses in leadership positions.
Making Health a ‘First Thought’
Donald Schwarz, MD, MPH, MBA, RWJF director, delivered the keynote address on building healthy communities. “We have a ways to go as a nation before health is a first thought, not a second thought,” he said. “Nurses have long led the way in saying that we need to care about more than just disease. How long and how well people live is central to nursing.”
Schwarz, who served as deputy mayor for health and opportunity and health commissioner in Philadelphia, described that city’s efforts to improve public health by providing and marketing healthier food options in corner stores and Chinese take-out restaurants, creating safer conditions for walking and bicycling, and raising penalties for tobacco sales to minors.
“Philadelphia shows what can be done to change the context,” Schwarz said. “You can do this. Nurses can be leaders in making changes where we live, work, and play.”
Julie Willems Van Dijk, PhD, RN, co-director of RWJF’s County Health Rankings & Roadmaps program, discussed how data can inform population health strategies. “There are many factors beyond health care services that affect lifespan and quality of life,” she said. “Because of nursing’s focus as relational, holistic practitioners, we stand in a perfect place to influence those factors on an individual and population level. There are tools and guidance available through County Health Rankings & Roadmaps to assist nurses in addressing population health.”
Working Together for a ‘Much Bigger Impact’
The meeting closed with a panel discussion on a new partnership between NJNI, NJAC, and New Jersey Health Initiatives (NJHI). All three organizations have support from RWJF, which is committed to improving health and health care in New Jersey and to strengthening the nursing workforce. NJNI, NJAC, and NJHI are collaborating on pressing issues, including redesigning nursing curricula, diversifying the state’s health care workforce, and preparing health care professionals to provide community-based care throughout the state.
“If we work together, we’ll have a much bigger impact,” said RWJF Program Officer Wendy Yallowitz, MSW. “It’s great to see this work happening in New Jersey.”
Yallowitz and other panelists—NJNI Program Co-Directors Salmond and Aline Holmes, DNP, RN, senior vice president for clinical affairs at the New Jersey Hospital Association; NJAC Co-Lead Cadmus; and NJHI Director Robert Atkins, PhD, RN, FAAN—discussed using school nurses and after-school programs to reach school-age children with messages about healthy lifestyles, how higher education can drive leadership in transforming health by giving academic credit for service learning, and ways to bolster community partnerships between health advocates, local governments, and faith-based organizations.
“We have to become more nimble and experimental,” Holmes said.
Dona Ortiz, RN, MSN, chief nursing officer at Meadowlands Hospital Medical Center, said she found the day’s sessions “really interesting and enlightening. What Dr. Schwarz did in Philadelphia, what Dr. Van Dijk is doing with county health data—that’s so informative to hear about. It gets you excited about all the possibilities.”
Back to Top
A Fond Farewell to the Collaborative Learning Community

- Diane M. Billings, EdD, RN, FAAN, ANEF, Director Faculty Preparation Program
The 2015 New Jersey Nursing Initiative (NJNI) annual meeting included a tribute to an important chapter in the program’s history: the Collaborative Learning Community (CLC), which was celebrated at a special gathering on the eve of the meeting.
When the Robert Wood Johnson Foundation (RWJF) launched NJNI in 2009, the CLC was created as an integral component of the Faculty Preparation Program. Since then, it has supported 61 New Jersey Nursing Scholars in their pursuit of master’s or doctoral degrees that qualify them for nurse faculty positions.
Through webinars, learning sessions, annual meetings, and an online network, the CLC not only supported NJNI’s goal to fuel the nurse faculty pipeline in New Jersey; it helped lay the groundwork for NJNI’s current focus on what and how nurse faculty teach the next generation of nurses.
NJNI Program Co-Director Susan W. Salmond, EdD, RN, ANEF, FAAN, executive vice dean and professor at the Rutgers School of Nursing, praised CLC Director Diane Billings, PhD, RN, chancellor’s professor emeritus at the Indiana University School of Nursing, for her contributions to the Faculty Preparation Program. “She’s been an integral part of the whole Scholar process,” Salmond said. “It’s amazing to see how involved she’s been in the lives of the Scholars.”
Because “Diane has been the star of the CLC program,” Salmond presented her with a certificate from the International Star Registry, showing that NJNI had named a star after Billings.
Over time, Billings said, CLC learning sessions and meetings were opened up to a broader audience than the Scholars the program supported, including nursing school faculty and health care administrators in the state. “I really feel we made an impact on deans and faculty, because we were talking about a new way to teach,” Billings said, “and as our Scholars finished their studies and came back into the nursing schools to teach, they’ve encountered an openness to new faculty input and new teaching strategies because we eventually included all faculty in our meetings. We’ve influenced many more people than the Scholars.”
Nanette Sulik, MSN, RN, CSN, a PhD Scholar at Rutgers, said, “The CLC made an incredible difference for me. Diane was absolutely amazing. I’ve taught for years, and the CLC has made me rethink things I’d taken for granted. I’ve been exposed to new practices and new points of view, and that has made me a better nurse educator.”
The gathering also provided an opportunity to recognize the final cohort of New Jersey Nursing Scholars. Five will receive their PhDs from Seton Hall University in May: Jeannie Couper, MSN, RN-BC; Lisa Heelan, MSN, FNP-BC, ANP-BC; Katherine Hinic, MS, APRN-BC; Patricia Ricci-Allegra, APN, CPNP; and Lori Wilt, MSN, RN, CSN. Five PhD Scholars at Rutgers are expected to finish their studies later this year: Ola Aloba, MSN, WHNP, APN; Donna Fountain, MA, MSN, APRN, PHCNS-BC; Emilia Iwu, RN, MSN, APN-C, FWACN; Sulik; and Mary Thomas, MSN, RNC.
Back to Top
Alumni and Scholars Update
- Alumna Tracy Perron, PhD, RN, CNE, CSN, and alumnus Robert Scoloveno, PhD, RN, CCRN, are working on two of the three $50,000 grants awarded by the New Jersey Nursing Initiative (NJNI) to nursing schools to plan pilot projects that bring academic and practice partners together on innovative curricular issues related to community-based care and promoting healthy lifestyles. Perron, an assistant professor at the College of New Jersey, is on the project team for the grant, “Using an Academic-Practice Partnership to Enhance Population-Focused Health Care in BSN Education: Planning for the Future.” Scoloveno, the simulation lab director and an assistant professor at Rutgers-Camden, is the project director for the grant, “Redesigning Nursing Education to Address the Challenges and Opportunities for Population Health.” These projects, along with one at Rutgers-Newark/New Brunswick that is focused on elder population health, will be considered for implementation grants for the 2015-16 academic year.
- Alumna Maria LoGrippo, PhD, RN, MSN, NE-BC, who teaches nursing at Rutgers and Seton Hall University, is continuing her work with the New Jersey Action Coalition (NJAC) as the project director for its Robert Wood Johnson Foundation Future of Nursing State Implementation Program grant. NJAC recently received a second round of funding to support and sustain its efforts to encourage nurses to continue their education and obtain bachelor’s or higher degrees.
If you are a New Jersey Nursing Scholar alumna or alumnus, or a current Scholar, please let NJNI know what’s new with you, so you can be featured in the next Alumni and Scholars Update section of the newsletter. Send your news about new jobs, research, publications, and more to info@njni.org.
Back to Top
Did You Know…?
- Marie Foley, PhD, RN, CNL, has been appointed dean of the Seton Hall University College of Nursing. Foley, also an associate professor at Seton Hall, has served as project director for the New Jersey Nursing Initiative (NJNI) Faculty Preparation Program at the university.
- National Nurses Week is May 6-12 and the theme this year is “Ethical Practice. Quality Care.” Let NJNI know what you’re doing in observance by tweeting with the hashtags #NursesWeek and #NJNI.
- NJNI has launched a new website at www.njni.org, featuring a fresh design, enhanced mobile device compatibility, and a Resources & Tools Library designed to support nurses and nurse faculty throughout their careers.
- The New Jersey Hospital Association hosted its annual Nurses in the Boardroom learning session on February 5. In addition to an overview of boardroom structure and competencies, this year’s session featured an in-depth discussion on health care finance and quality and patient safety. Robert Wood Johnson Foundation Senior Adviser for Nursing Susan B. Hassmiller, PhD, RN, FAAN, delivered the keynote address urging nurse leaders to apply their talents and expertise in boardroom settings. Learn about future sessions at www.njha.com/education.
- NJNI is active on social media, and wants to connect with you! Be sure to follow @NJNIprogram on Twitter, and keep up with NJNI on Facebook at www.facebook.com/NewJerseyNursingInitiative.
Back to Top
Feb 11, 2015 | Newsletter Archives
In this Issue:
New Jersey Summit Hits High Points in Academic Progression Journey
NJNI Begins New Pilot Project With Planning Grants
Alumni and Scholars Update
Did You Know…?
New Jersey Summit Hits High Points in Academic Progression Journey
Action Coalition Highlights Importance of Alliances with NJNI and others.

Speakers at the New Jersey Action Coalition Seamless Academic Progression Summit II included, from left, Marianne Markowitz, MS, RN, CNE, vice president and dean of St. Joseph’s College of Nursing, and Susan Bastable, EdD, RN, nursing department chair and professor at Le Moyne College, both in New York state, and Ann Hubbard, DNP, EdD, ARNP, CNE, associate dean of nursing at Indian River State College in Florida.
The New Jersey Action Coalition (NJAC) Seamless Academic Progression Summit II drew more than 60 attendees to hear local and national perspectives on advancing education transformation, a key recommendation in the landmark Institute of Medicine (IOM) report The Future of Nursing: Leading Change, Advancing Health.
After NJAC Co-Lead Edna Cadmus, PhD, RN, NEA-BC, FAAN, welcomed the crowd assembled at the New Jersey Hospital Association in Princeton in late November, she introduced Pat Polansky, RN, MS, co-director of the Center to Champion Nursing in America, an initiative of AARP, the AARP Foundation, and the Robert Wood Johnson Foundation (RWJF) that serves as national headquarters for the Future of Nursing: Campaign for Action. The Campaign is working to implement the IOM’s future of nursing recommendations through Action Coalitions it has created in all 50 states and the District of Columbia, and at the national level.
Polansky challenged attendees to view health care’s rapid evolution as a “race” that nurses must embrace. “If nurses don’t elevate and integrate,” she said, “we will remain mid-level providers.”
New Jersey Nursing Initiative (NJNI) Program Co-Director Susan Salmond, EdD, RN, ANEF, FAAN, executive vice dean and professor at the Rutgers School of Nursing, and Maria LoGrippo, PhD, RN, MSN, NE-BC, a New Jersey Nursing Scholar alumna and project director for NJAC’s academic-progression-focused State Implementation Program grant from RWJF, reported on NJAC’s Academic Progression Pilot Project.
“Education in New Jersey has a history of being siloed,” Salmond observed. “The changes we’re experiencing are very exciting—realizing that we’ve had to come out of our silos and work together. It’s fantastic to see the commitment to collegiality and collaboration in the state now.”
As the project shifts its focus from gap analysis to model design, LoGrippo said, priorities include alliances such as working with RWJF’s New Jersey Health Initiatives and NJNI programs; optimizing in-kind support from the New Jersey Hospital Association; providing “navigators” who will promote seamless academic progression models to both associate degree RNs and non-nurses in practice settings who are interested in pursuing bachelor of science in nursing (BSN) degrees; increasing diversity among aspiring nurses; and developing an online tool that provides guidance for students on nursing education and financial aid.
“We may not have consensus on one model in New Jersey,” LoGrippo added, “but we want there to be transparency about the models that do work.”
Mary Baroni, PhD, RN, professor of nursing and health studies at the University of Washington, Bothell, highlighted efforts to enhance curricular alignment between two- and four-year institutions and streamline a statewide associate degree in nursing (ADN)-to-BSN curricular pathway.
Sharon Gavin Fought, PhD, RN, director and associate professor of nursing at the University of Washington, Tacoma, and Gerianne Babbo, RN, MN, professor and associate dean for nursing at Olympic College, a two-year institution, shared their process for building an RN-to-BSN partnership. A crucial aspect, Fought said, was committing “to a new level of communication and trust. We had a lot of conversations that we were building on the ADN program, not replacing it. Now we don’t hear that concern anymore.”
Ann Hubbard, DNP, EdD, ARNP, CNE, associate dean of nursing at Indian River State College in Florida, discussed her institution’s successful online RN-to-BSN program, while Susan Bastable, EdD, RN, nursing department chair and professor at Le Moyne College, and Marianne Markowitz, MS, RN, CNE, vice president and dean of St. Joseph’s College of Nursing, talked about their efforts in New York state to establish a Dual Degree Partnership in Nursing.
“This model would not work without both partners,” Bastable said. “They can’t do it alone. One or the other is not going to disappear.”
“We can’t emphasize the importance of practice partners enough,” Markowitz added. “They’re crucial for clinical placements, and it’s important for them to recognize the value of these students.”
The summit also devoted time to a panel on workforce needs in acute care, home health nursing, and long-term care.
Magnet hospitals have been a driving force in increasing the number of nurses with BSNs, said panelist Robyn Begley, DNP, RN, NEA-BC, vice president of nursing and chief nursing officer for AtlantiCare Regional Medical Center. She added that with health care shifting away from acute care settings, “we are looking at innovative approaches across the continuum—hospice, telehealth, palliative care and more.”
Back to Top
NJNI Begins New Pilot Project With Planning Grants
Three nursing programs have been chosen to receive New Jersey Nursing Initiative (NJNI) Redesigning Nursing Education to Address the Challenges and Opportunities and Population Health Planning Grant Awards. Each grantee will receive $50,000 to plan a pilot project that brings academic and practice partners together on innovative curricular issues.
The grant recipients are:
- The College of New Jersey, Using an Academic-Practice Partnership to Enhance Population-Focused Health Care in BSN Education: Planning for the Future;
- Rutgers (Newark/New Brunswick), Redesigning Nursing Education to Address the Challenges and Opportunities of Elder Population Health; and
- Rutgers (Camden), Redesigning Nursing Education to Address the Challenges and Opportunities for Population Health.
These grantees will be considered for implementation grants for the 2015-16 academic year.
NJNI had a successful experience with earlier Innovations in Clinical Education pilot projects. This latest effort reflects NJNI’s shift from faculty preparation to faculty development, and its enhanced focus on encouraging nursing educators in the Garden State to transition curricula and clinical experience in order to help prepare nurses to meet the emerging demands of community-based care and population health.
Back to Top
Alumni and Scholars Update
- New Jersey Nursing Scholar alumna Maria LoGrippo, PhD, RN, MSN, NE-BC, was one of 10 recipients of the new Breakthrough Leaders in Nursing award created by the Future of Nursing: Campaign for Action, a joint initiative of AARP and the Robert Wood Johnson Foundation (RWJF). The award celebrates nurse leadership and the importance of efforts by nurses to improve health and health care.
LoGrippo, who teaches nursing at Rutgers and Seton Hall University and serves as project director for the New Jersey Action Coalition’s academic-progression-focused State Implementation Program grant from RWJF, and her fellow award recipients were recognized during the Campaign for Action Summit in November in Phoenix.
- Lisa Heelan, MSN, FNP-BC, ANP-BC, who is pursuing her PhD at Seton Hall University as a New Jersey Nursing Scholar, has given several presentations since the current academic year began. Her poster abstract, “Patient Advocacy: The Role of Research and Power to Participate Knowingly in Change,” was selected by Seton Hall for the Rising Stars in Nursing invited poster program at Sigma Theta Tau International’s Leadership Connection event, which was held in September in Indianapolis.
Also, Heelan’s abstract for the oral presentation “Human Dignity and Power in Childbirth” and her poster presentation “Human Dignity and Patient Advocacy as Mutual Process” were accepted by the Rogerian Society for a conference held in October in Knoxville, Tenn.
If you are a New Jersey Nursing Scholar alumna or alumnus, or a current Scholar, please let NJNI know what’s new with you, so you can be featured in the next Alumni and Scholars Update section of the newsletter. Send your news about new jobs, research progress, publications, and more to info@njni.org.
Back to Top
Did You Know…?
- The next Collaborative Learning Community (CLC) event is the February 12 webinar, Ongoing Professional Development: How to Bring Value to Your Organization, Community and Profession. The webinar will provide guidance on self-presentation and self-marketing, building a professional portfolio, effectively presenting that portfolio to various audiences, networking to build a career, building leadership skills, and more. It is intended to help Scholars prepare for their careers as leaders in nursing, research and academia.
- A CLC graduation event will be part of the New Jersey Nursing Initiative Annual Meeting on April 9 and 10. Stay tuned for additional details.
- The New Jersey Nursing Initiative (NJNI) is active on social media, and wants to connect with you! Be sure to follow @NJNIprogram on Twitter, and keep up with NJNI on Facebook at www.facebook.com/NewJerseyNursingInitiative.
Back to Top
Sep 22, 2014 | Newsletter Archives
In this Issue:
Curriculum Changes Emerge as a New Priority for NJNI
Deans and CNOs: Together by Design
Four N.J. Nursing Scholars Complete Advanced Degree Programs
A New Year for the Collaborative Learning Community
Alumni and Scholars Update
Did You Know…?
Curriculum Changes Emerge as a New Priority for NJNI
Over the past year since they were appointed co-directors of the New Jersey Nursing Initiative (NJNI), Aline M. Holmes, DNP, MSN, RN, and Susan W. Salmond, EdD, RN, ANEF, FAAN, have launched a new phase of the program’s work. Building on its legacy of faculty preparation, NJNI now focuses on faculty development and encouraging nursing educators in the Garden State to transition curricula and clinical experiences. Doing so will help prepare nurses to meet the emerging demands of community-based care and population health.
“Innovation is the key,” says Salmond, who is also executive vice dean of the Rutgers School of Nursing. “Career success for our graduates requires the state’s nursing programs to teach the relevant skills for the health care landscape of today and—more importantly—tomorrow.”
Several NJNI events this year, including a thought leaders’ summit, a conference of deans and chief nursing officers, and the annual meeting, have targeted hot topics relating to population health, the Triple Aim, interprofessional education, and partnerships between academia and clinical practice. NJNI will be supporting this shift in priorities through a request for proposals for up to eight planning grants that will receive up to $50,000 each to bring academic and practice partners together on innovative curricular issues.
“We’re trying to establish the idea that curriculum has to change,” says Holmes, DNP, MSN, RN, who is also the New Jersey Hospital Association’s senior vice president for clinical affairs. “Programs can’t prepare nurses for hospital jobs only.”
“Acute care is still the glamorous setting,” adds Salmond, “but skill sets have to reflect both acute care and population health.”
For example, Holmes explains, the vast majority of children are never hospitalized. “Yet nursing programs emphasize inpatient pediatrics, when there’s a pressing need to make sure nurses have the skills and confidence to practice where children are. Nurses need to be up to speed on issues like well-baby visits, immunizations, diabetes and substance abuse. Health care needs are changing very quickly.”
Salmond and Holmes see momentum for curricular evolution starting to build, especially since NJNI has started to provide what Holmes calls a “safe table” where leaders from academia and clinical practice can come together to talk about the direction health care is taking.
“We are excited about the conversations that are occurring and anticipate New Jersey programs will take a lead in influencing new and innovative curricula,” she says.
“Practice and education have a lot to do to get students where they need to be,” Salmond adds, “but we are absolutely optimistic that nurses will be leaders in where health care is going, if the curriculum changes happen.”
Reproduced with permission of the Robert Wood Johnson Foundation, Princeton, N.J.
Back to Top
Deans and CNOs: Together by Design

The New Jersey Nursing Initiative (NJNI) convened a Design Thinking Retreat in June at the Robert Wood Johnson Foundation, bringing together more than 60 nursing school deans, chief nursing officers, and key stakeholders as part of NJNI’s ongoing efforts to bring academic and practice leaders to work together to move nursing education forward.
The day-long retreat explored ideas for pilot projects geared toward population health objectives, and provided a forum for discussing gaps between nursing education and practice. Eight groups worked on designs for curricula, student experience, and faculty support and development that would prepare students for the future of population health.
Several common themes emerged, including:
- Interprofessional training and skill building;
- Increasing clinical experience;
- Clinical mentorship;
- Data and technology skills;
- Professionalism and patient engagement skills; and
- Increased specialization for nurses.
As participants reflected on the retreat, one wrote that “being able to sit together to share needs from both sides to improve what we both do is a win-win, especially when resources become tighter, both financial and human. More communication … will benefit the nursing profession and can really lead to positive future growth.”
Another pointed out the need for “easier access to other clients outside of acute care. A great deal of ‘community’ or ‘public health experience’ winds up being observational. How do we give our students meaningful experience when not in an acute care setting? Observation is a valuable tool in learning, but hands on enhances the learning much more.”
“We have many goals but need to work together,” wrote another participant. “We need access to services, fewer barriers to practice, support onward to share resources, and human resources to improve population health outcomes.”
NJNI has incorporated ideas exchanged at the retreat into an upcoming request for proposals for pilot projects that bring academic and practice partners together on innovative curricular issues.
Back to Top
Four N.J. Nursing Scholars Complete Advanced Degree Programs
With the support of the New Jersey Nursing Initiative (NJNI), four more highly educated nurses are prepared to assume faculty roles and help meet the educational needs of New Jersey’s nursing workforce in a rapidly evolving health care landscape.
Three of NJNI’s Faculty Preparation Program participants, known as New Jersey Nursing Scholars, recently completed their doctorates at the Rutgers School of Nursing:
- Shanda Johnson, PhD, MS, RN, APN-C, FNP, of Scotch Plains;
- Aleesa M. Mobley, PhD, RN, APN-C, of Williamstown; and
- Catherine Jirak Monetti, PhD, MA, RN, of Mountain Lakes.
One scholar earned her master’s degree at the Rutgers School of Nursing:
- Karon Branch, MSN, RN, FNP, of Willingboro.
Additionally, Jenee Skinner-Hamler, DNP, RN, FNP, of Mays Landing, who had completed her master’s degree at the Rutgers School of Nursing in 2011 as a New Jersey Nursing Scholar, received alumni incentive funding from NJNI and completed her doctor of nursing practice degree at Wilkes University in Wilkes-Barre, Pa.
The Robert Wood Johnson Foundation launched NJNI in 2009, and it has now supported 51 New Jersey Nursing Scholars who have completed master’s or doctoral degrees qualify them for nurse faculty positions. NJNI’s final cohort of scholars—10 PhD students—continue in their programs.
“The New Jersey Nursing Scholars are a vital part of NJNI’s legacy, and a reflection of its future,” said NJNI Program Co-Director Susan W. Salmond, EdD, RN, ANEF, FAAN. “We’re proud to help fuel the pipeline of nurse faculty needed to educate the next generation of nurses.”
“NJNI’s initial focus on the state’s nurse faculty shortage has helped us better understand where to go next,” added NJNI Program Co-Director Aline M. Holmes, DNP, MSN, RN. “Now we’re encouraging the state’s nursing programs to teach the relevant skills that will help students succeed in meeting emerging health care needs.”
“Without the support of the Robert Wood Johnson Foundation and the New Jersey Nursing Initiative, the prospect of pursuing doctoral studies was daunting,” said Monetti. “This experience gave me so much more than teaching credentials.”
Mobley, who holds an adjunct faculty position at Rowan University and is pursuing a full-time tenure-track position there, said that NJNI “encouraged and enhanced better teaching skills. I plan on giving my professional best in return.”
“I’ve always loved the profession, and I’m eager to teach other nurses in the future,” said Branch, a family nurse practitioner who hopes to become a primary care provider and teach part time.
Johnson, a family nurse practitioner who plans to teach part time this fall, said that the scholarship supported her research on adolescent obesity, enhancing both her clinical and academic skills. “I’d like to eventually serve as a dean or in a similar leadership role,” she said. “It’s important to have nurses in those positions.”
NJNI’s priorities now include:
- An Online Faculty Development Program;
- Enhanced partnerships with other organizations, including a key role with the New Jersey Action Coalition, which helps the Future of Nursing: Campaign for Action implement recommendations from the Institute of Medicine’s landmark 2010 nursing report as part of a nationwide effort to transform nursing and the delivery of health care in America;
- Promoting educational initiatives and pilot projects that will attune nursing education to community-based and population health; and
- Encouraging curricular and instructional changes in nursing to better reflect health care trends.
Back to Top
A New Year for the Collaborative Learning Community
The Collaborative Learning Community (CLC) will get underway for the new academic year with a conference on October 10 at the Robert Wood Johnson Foundation: “Health Care in the Community: Developing Academia/Practice Partnerships for Care Coordination and Managing Care Transitions.”
The session will focus on health care’s shift from inpatient to outpatient settings, where care coordination and accountability can be challenging. The presentation will identify the dimensions of care coordination and transition management; describe the associated competencies, including knowledge, skills and attitudes; and offer strategies to educate nursing students in support of developing team-based collaborative ambulatory practice environments that deliver quality and safe care that is patient- and population-centered.
NJNI congratulates two CLC participants who have recently been inducted as Fellows of the American Academy of Nursing: Karen D’Alonzo, PhD, RN, APN-C, and Tony Forrester, PhD, RN, ANEF, both of whom are professors at the Rutgers School of Nursing. D’Alonzo is NJNI’s Faculty Preparation Program director at Rutgers, and Forrester has served as a panelist and presenter for several CLC sessions.
Back to Top
Alumni and Scholars Update
- Rahshida Atkins, PhD, APN, FNP-BC, is doing postdoctoral research at the University of Pennsylvania.
- Karon Branch, MSN, RN, FNP, attended a learning session, Nurses in the Boardroom, hosted by the New Jersey Hospital Association. The program was designed to engage nurses in assuming leadership roles on advisory and governance boards, where policy decisions that impact health care are made. Maryjoan Ladden, PhD, RN, FAAN, senior program officer at the Robert Wood Johnson Foundation, was the guest speaker.
- Emilia Iwu, MSN, RN, APN-C, FWACN, PhD(c), has received the 2014 Global Nursing Research Grant from Sigma Theta Tau International for her dissertation research proposal, “Shifting HIV Management Tasks from Physicians to Nurses in Africa.”
- Tracy Perron, PhD, RN, CNE, CSN, has been named an assistant professor at the College of New Jersey.
If you are a New Jersey Nursing Scholar alumna or alumnus, or a current Scholar, please let NJNI know what’s new with you, so you can be featured in the next Alumni and Scholars Update section of the newsletter. Send your news about new jobs, research progress, publications, and more to info@www.njni.org.
Back to Top
Did You Know…?

Edna Cadmus, PhD, RN, NEA-BC, FAAN, clinical professor at the Rutgers School of Nursing, has been appointed executive director of the New Jersey Collaborating Center for Nursing (NJCCN). Cadmus has more than 30 years of clinical and administrative experience and has been the recipient of numerous awards. Her extensive background in leadership positions includes: co-lead of the New Jersey Action Coalition, past president and current board member of ONE/NJ, and current vice chair-commissioner for Pathways to Excellence, American Nurses Credentialing Center. She is the specialty director for the graduate leadership tracks at Rutgers University. Learn more about NJCCN at www.njccn.org.
Back to Top
May 22, 2014 | Newsletter Archives
In this issue:
The Future Unfolds at NJNI’s Annual Meeting
Ideas Worth Exploring: NJNI’s First Thought Leaders Summit|
Journeys Continue for Two ICE Pilots
Action Coalition Update: E-Newsletter Launches, and More
Did You Know…?
The Future Unfolds at NJNI’s Annual Meeting

Nursing scholars, mentors, educators, and other health care leaders took their seats at the Robert Wood Johnson Foundation (RWJF) for two days in March for the 2014 New Jersey Nursing Initiative (NJNI) Anuual Meeting. But standing still, it was clear, was not an option.
From the meeting’s theme, Fast Forward: Shaping Nursing Education and Practice in the 21st Century, to the messages offered by the speakers, attendees were encouraged to let go of the status quo and lead the way in navigating New Jersey’s rapidly evolving health care landscape. They also had a shining example of adaptability in NJNI itself.
When RWJF launched NJNI in 2009, the program focused on fueling the nurse faculty pipeline in the Garden State so that there will be enough educators to teach the next generation of nurses. Today, with accomplishments that include supporting 61 New Jersey Nursing Scholars in their pursuit of master’s or doctoral degrees that prepare them for nurse faculty roles, NJNI has a new priority: encouraging the state’s nursing programs to teach the relevant skills that will help students succeed in meeting emerging health care needs.
“Some things haven’t changed since I was a student in the ’60s and ’70s,” NJNI Program Co-Director Susan W. Salmond, EdD, RN, ANEF, told attendees as the meeting got underway. “We have to prepare nurses for the new world of health care. That’s why we’re here.”
Since they were appointed last year, guiding NJNI into a new phase has been a priority for Salmond, who also serves as dean of the Rutgers School of Nursing, and for Program Co-Director Aline M. Holmes, DNP, MSN, RN, who is also the New Jersey Hospital Association’s senior vice president for clinical affairs. The Initiative’s priorities now include an Online Faculty Development Program; enhanced partnerships with other organizations; promoting educational initiatives and pilot projects that will attune nursing education to community-based and population health; and encouraging curricular and clinical pedagogical changes in nursing to better reflect emerging and future health care trends.
‘We Have to Look Outward’
George E. Thibault, MD, president of the Josiah Macy Jr. Foundation, was one of several speakers at the meeting who reinforced NJNI’s focus on synchronizing nursing academics and practice. “We won’t have enduring reform without changes in education,” he said. “We’ve used a curriculum derived from academic leaders’ heads. Instead of looking inward, we have to look outward. Have we achieved societal goals, not just curricular goals? That’s a paradigm shift.”
In his keynote address, noted consultant James E. Orlikoff, MA, emphasized the stark economic realities of health care that make change inevitable. “We cannot afford the product we are producing,” he said. “What does that mean? Reduce your cost or go out of business.”
Judith F. Karshmer, PhD, PMHCNS-BC, dean of the School of Nursing and Health Professions at the University of San Francisco, and Kathleen Gallo, PhD, MBA, RN, FAAN, senior vice president and chief learning officer at North Shore-LIJ Health System, both highlighted the need for disruptive innovation in education. Gallo zeroed in on the importance of interprofessional education and team-based care, while Karshmer discussed several academic areas ripe for rule-breaking, especially the standard approach to nursing competencies.
“We must stop treating hours of clinical time as equal,” Karshmer said. “It’s not about the hours, it’s about the competency. We have to rethink what the competency is. Right now, it’s like telling a patient, ‘You got healthy in two days, but you have to stay for four.’ That’s how we’re treating competency-based education.”
The Spirit of Collaboration
NJNI devoted the second day of the meeting to the Collaborative Learning Community (CLC), originally scholar-focused but now expanded to include a broader audience, explained CLC Facilitator Diane Billings, EdD, RN, FAAN.
Robyn Begley, DNP, RN, NEA-BC, chief nursing officer at AtlantiCare Regional Medical Center, discussed trends and challenges in nursing, including the shift from acute to chronic and primary care; the shift to population care; and overcoming barriers to change. “I believe the future is very bright for nurses,” she said.
She was followed by Susan Hendricks, EdD, RN, CNE, the associate dean for undergraduate programs at the Indiana University School of Nursing, whose message to current and aspiring faculty was that “we can’t afford to be behind change. We have to get in front of it.”
“Everyone owns curriculum,” Hendricks added, “not just the few people who’ve traditionally developed it.”
Thinking Outside of Silos
As the meeting wound down, Hendricks said that she was happy to not only have shared her perspective, but to be taking away new ideas as well. “There are a number of leaders in New Jersey who are poised to move the state and the nation forward,” she said. “It was great to see a lot of people from practice engaging during the meeting, and there weren’t just questions put out there. There were some answers, too. This is what needs to happen—academia and practice sitting side by side.”
Marie Foley, PhD, RN, chair of the Graduate Department at the Seton Hall University College of Nursing, agreed. “It’s wonderful to have the perspective of practice,” she said. “The whole economic piece was fantastic. So eye-opening. We don’t often hear that. We have to look outside of our silos, and the meeting really reinforced that.”
In her parting words to attendees, Holmes said, “It’s been a great couple of days with very creative ideas. I challenge you all to go home and put these ideas into action.”
Back to Top
Ideas Worth Exploring: NJNI’s First Thought Leaders Summit

Attendees at the NJNI Thought Leaders Summit meeting in February 2014 included, clockwise from left, NJNI Program Co-Director Aline Holmes; CFAR consultant Carey Gallagher; Executive Director NJ Board of Nursing George Hebert; NJNI Program Co-Director Susan Salmond; NYU Director of Education and Program Development Linda Bub; CNO/COO NYU Medical Center Margaret McClure; CFAR Consultant Jennifer Tomasik; North Shore LIJ Chief Learning Officer Kathleen Gallo; CareCam Health Systems Chief Clinical Officer Sandra Ryan; Thomas Jefferson University, School of Nursing Dean and Professor Beth Ann Swan; Aetna Vice President and National Medical Director Medical Strategy Randall Krakauer; RWJF Senior Program Officer Maryjoan Ladden; NJNI Program Coordinator Nina Raoji; Visiting Nurse Service of New York President and CEO Mary Ann Christopher; Rutgers University Director of DNP Leadership Program Edna Cadmus; NJHA Vice President Post- Acute Care Policy & Special Initiatives Theresa Edelstein; Mississippi Hospital Association HRET President/CEO Marcella McKay; NJNI Projects Coordinator Hazelene Johnson; Jersey City Medical Center ACO Vice President Community Medicine Susan Walsh; NJNI Deputy Director Jennifer Polakowski. Attendees not pictured above include Meridian Health Vice President of Clinical Integration Maureen Bueno; Robert Wood Johnson University Hospital Director of Clinical Integration Lois Dornan; Princeton University Director of State Health Reform Implementation Program Heather Howard; PR Solutions Consultant Jonathan Padget.
As part of its transition into a new phase, the New Jersey Nursing Initiative (NJNI) held its first Thought Leaders Summit in February at the Robert Wood Johnson Foundation. The Summit provided an opportunity for brainstorming and discussion on a number of ways NJNI can tackle pressing challenges. The ideas exchanged will undoubtedly influence future pilot projects. NJNI is grateful to the following participants for sharing their time and expertise:
Linda Bub, MSN, RN, GCNS-BC, director of education and program development at New York University College of Nursing’s Nurses Improving Care for Healthsystem Elders program;
Maureen Bueno, PhD, RN, vice president for clinical integration at Meridian Health;
Edna Cadmus, PhD, RN, NEA-BC, FAAN, professor and director of the doctor of nursing practice leadership program at the Rutgers College of Nursing;
Mary Ann Christopher, MSN, RN, president and chief executive officer of the Visiting Nurse Service of New York, and NJNI national advisory committee chair;
Lois Dornan, MSN, RN, CPHQ, director of clinical integration at Robert Wood Johnson University Hospital;
Theresa Edelstein, MPH, LNHA, vice president for post-acute care policy and special initiatives at the New Jersey Hospital Association;
Kathleen Gallo, PhD, MBA, RN, FAAN, senior vice president and chief learning officer at North Shore-LIJ Health System;
George Hebert, MA, RN, executive director of the New Jersey Board of Nursing;
Heather Howard, JD, BA, director of the State Health Reform Assistance Network and lecturer in public affairs at Princeton University, and NJNI national advisory committee member;
Randall Krakauer, MD, national medical director at Aetna;
Margaret McClure, RN, EdD, FAAN, professor at New York University and former chief nursing officer and chief operating officer at New York University Medical Center;
Marcella McKay, PhD, MSN, MEd, RN, chief operating officer of the Mississippi Hospital Association, president and chief executive officer of the Mississippi Hospital Association Health, Research & Educational Foundation, and NJNI national advisory committee member;
Sandra Ryan, MSN, CPNP, FCPP, FAANP, FAAN, chief clinical officer at CareCam Health Systems;
Beth Ann Swan, PhD, CRNP, FAAN, dean and professor at Thomas Jefferson University; and
Susan Walsh, MD, vice president for community medicine and accountable care organization medical director at Jersey City Medical Center.
Also at the Summit, eight thought leaders participated in video interviews, answering four questions about the direction of nursing and its importance. The videos will be featured later this year on NJNI’s website. Here are four excerpts that capture the spirit of the conversations.
What is the greatest challenge that needs to be tackled in nursing education today, in order to help nurses succeed in the health care landscape of tomorrow?
As a geriatric clinical nurse specialist, I think the greatest challenge in nursing education is identifying and meeting the needs of the older adult. Integrating geriatrics into programs, transitions of care for this population, working with long-term care, assisted living, and home care—we really have to broaden the range of nursing practice outside of the acute care setting. —Linda Bub
As people talk about the evolution of nursing and health care, and what it will take to move forward, are there issues that haven’t come up yet or that need to be emphasized more?
The future of nursing is going to be extraordinarily independent. It’s clear that there are not going to be as many jobs in inpatient settings. But inpatient settings provide students and brand-new nurses with the opportunity to practice in situations where they have people to turn to for help. The community setting is much different when it comes to learning. We have to plan for this more autonomous setting.—Margaret McClure
How different will nursing, and nursing education, look 10 years from now?
The hope would be that in 10 years, it’s the same in the sense that we’re still teaching nurses how to be a key part of our health care system. But it’s different in the sense that we’re teaching them to prevent, treat, and manage chronic diseases, and teaching them how to be a critical part of promoting population health.—Heather Howard
Why does nursing matter to you, and how do you see yourself moving nursing forward?
Nursing matters to me tremendously on many different levels. It’s a profession that’s grounded in patient-centeredness, and making sure the right things are done for the patient, in the right context. Also, because of my own path toward becoming a chief clinical officer for a mobile health technology company, I find it amazing how the boundaries in nursing are coming down. Nurses need to look at how they can play a bigger-picture role and have influence across all sectors, and I will continue to work on having a positive influence in people’s lives.—Sandra Ryan
Back to Top
Journeys Continue for Two ICE Pilots
NJNI’s Innovations in Clinical Education (ICE) program included four pilot projects, one of which has been sustained since the program concluded more than a year ago. “We’ve continued basically all aspects of the project,” said Minerva Guttman, EdD, RN, NP, director of the nursing school at Fairleigh Dickinson University (FDU). FDU’s participation in the ICE program included partnering with Holy Name Medical Center on preceptor strategies for community health nursing and hospice care.
“The nurses really enjoyed it, and we saw that it was making a difference. The student evaluations show they’re learning a lot,” Guttman continued.
To sustain the project, she said, the university incorporated preceptor training into the workload of the community health nursing faculty. Also, preceptors qualify for free tuition in RN-to-BSN and master’s programs. “It’s a good model that’s working well for us,” Guttman added.
Another ICE pilot will soon share its dedicated education unit (DEU) experience with a national audience. Julie Bliss, EdD, RN, chair of the William Paterson University Department of Nursing, which partnered with St. Joseph’s Regional Medical Center, has written an article that will be published in conjunction with a July conference celebrating the 10th anniversary of the Portland Model DEU, considered by many experts to be an exemplary model for preparing the next generation of nurses.
Back to Top
Action Coalition Update: E-Newsletter Launches, and More
The New Jersey Action Coalition (NJAC), which helps the Future of Nursing: Campaign for Action implement recommendations from the Institute of Medicine’s landmark 2010 nursing report, is now publishing an e-newsletter that provides quarterly updates on NJAC’s progress, as well as important nursing news. The goal of the Campaign’s work is that everyone in America can live a healthier life, supported by a system in which nurses are essential partners in providing care and promoting health. View the NJAC newsletter online at www.njactioncoalition.com, and sign up to receive it directly by sending a request to info@njactioncoalition.com.
NJAC also invites nurses to visit its website to share their stories about how they are contributing to health care’s transformation through one of the Institute of Medicine’s Future of Nursing recommendation areas: expanding scope of practice, advancing education, leadership, and workforce data. Selected stories will be featured online and shared with Action Coalition partners across the nation.
Additionally, NJAC is recruiting speakers to give presentations on its work, and needs to know if there are nurse leaders who’ve recently taken on board roles. Contact info@njactioncoalition.com to learn more about speaking opportunities, and to share any updates.
Back to Top
Did You Know…?

May brings a milestone for NJNI Program Co-Director Aline Holmes, DNP, MSN, RN,
who received her doctor of nursing practice degree from the Rutgers College of
Nursing. “It was on my bucket list,” she recently told Rutgers Today. “And I figured if
I am going to help transform nursing education, I should walk the walk.”
– NJNI is piloting six faculty development modules with current scholars and alumni: Meeting the Challenges of the Educational System as a New Faculty; Transitioning to a Tenure-Track Position at a Research-Intensive University; Effective Teaching Strategies; Evidence-Based Teaching; Civility in the Academic Environment; and Online Learning in Nursing Education. NJNI plans to introduce a sustainable, comprehensive Online Faculty Development Program that will support the needs of up-and-coming New Jersey nurse faculty.
– If you are a New Jersey Nursing Scholar alumna or alumnus, please let NJNI know what’s new with you, so you can be featured in the next Alumni Update section of the newsletter. Send your news about new jobs, research progress, publications, and more to info@www.njni.org.
Back to Top
Dec 16, 2013 | Newsletter Archives
In This Issue
NJNI’s Future Takes Shape at National Advisory Committee Meeting
NJNI Scholar Helps Address Social Isolation Among the Mentally Ill
Alumni Update
Collaborative Learning Community Gets Underway for 2013-2014
Did You Know..?
NJNI’s Future Takes Shape at National Advisory Committee Meeting

Attendees at the NJNI national advisory committee (NAC) meeting in October 2013 included, clockwise from left, NAC members Heather Howard and Susan Walsh; NJNI Program Director Susan Salmond; NAC members Dana Egreczky, Arnold Speert, Sonia Delgado, Ruben Fernandez, and Peter Inverso; NJNI Deputy Director Jennifer Polakowski; NAC Chair Mary Ann Christopher; RWJF Senior Program Officer Maryjoan Ladden; and NJNI Program Director Aline Holmes. Also serving on the NAC are Catherine Alicia Georges, Penelope Lattimer, Marcella McKay, Mary Sibley, and Mary Wachter.
Leaders of the New Jersey Nursing Initiative (NJNI) gathered in October at the Robert Wood Johnson Foundation (RWJF) to discuss what the future holds for the Initiative in its “NJNI 2.0” phase.
Newly appointed program directors Aline M. Holmes, MSN, RN, and Susan W. Salmond, EdD, RN, ANEF, FAAN, were joined by members of the national advisory committee (NAC) for the day-long meeting. It was devoted to strategic planning as NJNI builds on its support for 61 New Jersey Nursing Scholars who are pursuing, or have completed, master’s or doctoral degrees at nursing programs in the state. They are now poised to assume nurse faculty roles in New Jersey.
RWJF and the New Jersey Chamber of Commerce Foundation launched NJNI in 2009 to address the state’s nurse faculty shortage and help avert the projected shortage of more than 23,000 nurses in New Jersey in less than two decades.
NAC Chair Mary Ann Christopher, MSN, RN, FAAN, welcomed attendees, who were then introduced to Holmes and Salmond by RWJF Senior Program Officer Maryjoan D. Ladden, PhD, RN, FAAN, setting the stage for the program directors and their deputy, Jennifer Polakowski, MPA, to lead a discussion of NJNI 2.0 priorities, including:
- Communications efforts such as a website redesign and social media outreach;
- A toolkit for the Faculty Preparation Program that disseminates lessons learned;
- A Faculty Development Program that can provide sustainable professional development opportunities for nurse faculty in New Jersey;
- Enhanced partnerships with other organizations to advance NJNI goals; and
- Academic leadership that will attune nursing education to community-based and population health.
“What skills do nurses need now, and five years from now?” Holmes asked. “We’re figuring out dedicated education units, but we need to figure out how to create community education units, because that’s where so many nurses are going to be practicing.”
“We’re embracing the reality of health care,” Salmond added. “What does nursing education need to do? We’re teaching in traditional ways. As an educational community in New Jersey, NJNI needs to lead the shift to the educational needs of tomorrow, which is already here today.”
NAC members weighed in with expert perspectives on a number of topics, including efficiency and safety issues, interdisciplinary approaches to care, new core competencies for front-line nurses, cultural dimensions of care, encouraging a more responsive regulatory system, and incorporating leaders from the insurance industry and other business fields into NJNI’s work.
“Ultimately, we want to create a brain trust to look at all of these issues and help move nursing to a new realm,” said Salmond.
After the meeting, Christopher said she sensed “a lot of momentum from the group. All of the ideas discussed represent an opportunity to transform the health care system at a time when it’s critically important to do so.”
NAC member Sonia Delgado, MGA, said, “It was exciting to see people thinking outside of the box, getting ahead of the curve, and thinking about the value nurses bring to health care. I’m glad that people understand the need to think big.”
“The group was engaged on bridging the gap between academia and practice, and developing new competencies,” Holmes said. Salmond added, “There was recognition that the future is a different health care world. We’re going to have to redesign education. We want to build on the past and look at where nursing education must be.”
Ladden called the NJNI 2.0 objectives “a perfect next step. They build on what NJNI did with the Faculty Preparation Program, and really take the Initiative where it needs to go.”
Back to Top
NJNI Scholar Helps Address Social Isolation Among the Mentally Ill
Front-line experience leads RWJF Scholar to warn that failing to focus on social integration and interaction may put mental health patients at risk.
“People with mental illness have much more going on in their lives than just their mental illness.”
It was a realization Sheila Linz had early in her nursing career, she said, because she spent many years working closely with people struggling with severe cases of schizophrenia, bipolar disorder, and other mental health problems. But as the treatment system shifted its emphasis from institutional settings to independent living, Linz, PhD, PMHNP-BC, RN, began to worry that a critical component of mental health was getting lost along the way: social interaction.
That concern led her to choose social isolation in the severely mentally ill as her research focus when she started her PhD program at Seton Hall University as a Robert Wood Johnson Foundation New Jersey Nursing Initiative (NJNI) New Jersey Nursing Scholar.
“When I was younger, I worked in a facility where a lot of people lived, and we had social groups, entertainment, and things for people to do on weekends,” Linz recalled. “But the model is moving away from that. People like to live in their own apartments, and it’s also more affordable. As a nurse and a nurse practitioner, I went into the homes of people with severe mental illness, and they looked very lonely to me. They would always be sitting in their apartments, watching television by themselves. It seemed to me that this was not good for their mental health, and it also left a whole lot more time for their delusions and for responses to their voices.”
Midway through her PhD work, Linz collaborated with Bonnie A. Sturm, EdD, RN, an associate professor of nursing at Seton Hall University, on “The Phenomenon of Social Isolation in the Mentally Ill,” a paper that consolidates a number of scholarly perspectives and analyses. It was published in the October issue of Perspectives in Psychiatric Care.
“In one way, more people are getting services, because you’re bringing services to the home,” said Linz, who graduated in May—among the first group of New Jersey Nursing Scholars to complete their PhD programs—and now teaches at Seton Hall. “But because of that, people don’t have any real need to leave their homes. There was a situation being created that I thought was pretty serious, especially since it’s so difficult for people with mental illness to be accepted into any kind of community activity, because there’s so much stigma about mental illness.”
A Link Between Social Isolation and Physical Health
Linz said her PhD work was also shaped by research showing that people with severe mental illness live 25 years less, on average, than the general population. “And this was not because of suicide,” she said. “There were a lot of metabolic disorders, and it could not be explained totally by their medications. I also saw that there was a lot of research about the general population having early morbidity and mortality due to social isolation. A lot of studies showed that social isolation was as much of a predictor of mortality, or a risk factor, as smoking or drinking.”
“I came to see social isolation as a problem not only affecting mental health, but also physical health, which is another huge problem,” Linz said.
The paper offers solutions, and describes the implications of implementing them for nursing practice. “It talks about successful methods to help people with severe mental illness engage with the outer world and have a better sense of who they are,” Linz said. “There are also suggestions for what the practitioner can recommend, such as volunteering, or seeking out activities, like art classes or poetry readings, that engage the patients around their interests and their cultural identification.”
“A lot of people with severe mental illness don’t even think they’re sick,” Linz added. “Those are the people who don’t go to medical appointments and end up homeless, or they’re back and forth between hospitals. These are the people who have treatment teams going to their homes. For them, there isn’t enough value placed on the role of social interaction and social integration in the healing of mental illness.”
Much of the information in the paper became part of Linz’s literature review for her dissertation, which explored how the problem of social isolation manifested itself in a group of people being served by the mental health care delivery system known as assertive community treatment, or ACT.
“These are multidisciplinary teams, including a nurse, and the team meets every morning to discuss each of their clients before individually going to the clients’ homes,” Linz said. “These teams have done well keeping people out of the hospital, but there are areas such as social integration where they have not done as well. It’s not a priority.”
Speaking to workers on seven different ACT teams from three agencies in two states gave Linz “a front-line perspective on how they define social integration, how they facilitate it, the barriers they face, how they overcome barriers, and what their own ideas are about ways the model could be changed. I got a lot of very interesting information.”
Read the study. Learn more about the New Jersey Nursing Initiative.
Reproduced with permission of the Robert Wood Johnson Foundation, Princeton, N.J.
Back to Top
Alumni Update
Welcome to the first installment of the new Alumni Update feature. Here’s what several New Jersey Nursing Scholars have been doing since graduation:
- Tony Malek (2012 alumnus), MSN, RN, CBN, is working in Newark at Beth Israel as an observation unit nurse practitioner to expedite discharge and lower 30-day readmission rates. He recently attended the American Association of Nurse Practitioners leadership conference in Las Vegas.
- Tracy Perron (2013 alumna), PhD, MSN, RN, published an article, “Peer Victimization: Strategies to Decrease Bullying in Schools,” in the February issue of the British Journal of School Nursing. She also worked with the New Jersey State Nurses Association on presentations in May about the impact of the state’s new anti-bullying law on school nursing, and served over the summer with Collaborative Learning Community Facilitator Diane Billings, EdD, RN, FAAN, on a Sigma Theta Tau International task force on faculty skills development programs.
- Shelby Pitts (2012 alumna), MSN, RN, has a full-time faculty position in Newark at Rutgers School of Nursing. She is teaching Community Health Nursing and Foundations.
- Latoya Rawlins (2011 alumna), MSN, RN, served as a panelist for the Collaborative Learning Community webinar on choosing a doctoral program. She is pursuing a doctor of nursing practice degree at Rutgers School of Nursing.
If you are a New Jersey Nursing Scholar alumnus, please let NJNI know what’s new with you, so you can be featured in an upcoming issue of the newsletter. Send your news to Deputy Director Jennifer Polakowski via email:info@www.njni.org.
Back to Top
Collaborative Learning Community Gets Underway for 2013-2014
NJNI’s Collaborative Learning Community (CLC), facilitated by Diane Billings, EdD, RN, FAAN, has gotten off to a busy start in the new academic year, with webinars on promoting a spirit of inquiry in academic nurse educators, choosing a doctoral program, and workplace bullying, as well as a two-day workshop devoted to the National League for Nursing Certified Nurse Educator (CNE) exam.
“It’s exciting that the CNE workshop was open to broader audiences—scholars, faculty, and university leaders,” Billings said during a break between sessions, held in October at RWJF.
Presentation materials from the fall webinars are available online. The next CLC event will be a workshop on integrating nursing informatics into the curriculum. The workshop will be held on February 7, 2014, from 9 a.m. to 4 p.m. at RWJF.
CLC participants should also mark their calendars for webinars on March 7 (technology in learning) and April 23 (helping the “challenging student”), as well as NJNI’s annual meeting, March 12-14 at RWJF, which will include a CLC session on curriculum redesign.
Back to Top
Did You Know..?
NJNI has a key role in the New Jersey Action Coalition (NJAC), which helps the Future of Nursing: Campaign for Action implement recommendations from the Institute of Medicine’s landmark 2010 nursing report as part of a nationwide effort to transform nursing and the delivery of health care in America.
NJAC recently announced that it has received funding of $1.6 million from the Centers for Medicare and Medicaid Services (CMS) to develop, implement, and evaluate an RN transition-into-practice residency model for long-term care (LTC) facilities in New Jersey. Working with the Health Care Association of New Jersey and volunteers from NJAC’s education pillar, NJAC will recruit 50 preceptors and 50 new nursing graduates for this 12-month residency.
NJAC hopes that the effort will improve care for LTC residents and help stabilize the state’s RN workforce. New Jersey’s readmission rates for geriatric adults with chronic diseases are among the highest in the country, and the 2010 turnover rate for staff nurses in New Jersey LTC facilities was 37.7 percent—higher than in other sectors of health care.
NJAC co-lead Edna Cadmus, PhD, RN, NEA-BC, FAAN, and NJNI Program Director Susan W. Salmond, EdD, RN, ANEF, FAAN, who is also co-chair of NJAC’s education pillar, will serve as co-investigators for the residency project, with the Rutgers College of Nursing in Newark taking the lead in overall management of the CMS funding.
“With a prestigious interdisciplinary team, along with others who will be participating with us over the next 30 months, we are excited about the impact we can make for long-term care residents in New Jersey,” Salmond said.
Learn more about NJAC online.
Back to Top
 On September 21, Katherine Hinic, RN, PhD, (Seton Hall University 2015), presented her dissertation research, “The Relationships Among Perceived Stress, Birth Satisfaction, and Breastfeeding Self-Efficacy in Early Postpartum Women,” at Morristown Medical Center’s Nursing Research Day.
On September 21, Katherine Hinic, RN, PhD, (Seton Hall University 2015), presented her dissertation research, “The Relationships Among Perceived Stress, Birth Satisfaction, and Breastfeeding Self-Efficacy in Early Postpartum Women,” at Morristown Medical Center’s Nursing Research Day.